To search this Diabetes Topics Catalogue, hold "Ctrl" + "f" (PC) or "Cmd" + "f" (Mac) and type in your search word. If problem opening PDFs, right click on the document, "save as" and save to desktop.
CONSIDER GIVING ALL YOUR PATIENTS THE Diabetes Resources in Calgary.PDF- click here.Diabetes Resources for Patients (diabetes phone-lines, classes, urgent help, routine 1:1 help). Diabetes Resources in Calgary.PDF- click here.Diabetes Resources for Patients (diabetes phone-lines, classes, urgent help, routine 1:1 help).
AHS - Misc Documents & Sites
- Consent-Authorizing a Representative
- DON SCN Documents & Resources
- MyHealth Records Portal for patients to review lab results and other information
- Patient and Caregiver Journal can be found on this AHS page. (Includes checklists of questions for patients to ask when referred to specialists).
Apps (diabetes related), Reports, Passwords
Numerous apps are available to assist those with diabetes. See the heading COMPUTER below if your patient needs help accessing the internet, has no internet or no computer. These include apps from companies for specific glucose meters, sensors, insulin pumps as well as third party apps. Most allow patients to view data and/or send reports from the app or from an online cloud service directly to their clinicians. It's important for eduators to direct patients to send reports, since not all health authorities have the approval to use "Clinic" clouds (e.g. an online server for the clinician/program that stores the glucose data of just their patients.)
Forgotten App Passwords for Glucose Data:
- If on iPhone under phone settings > passwords > search the app name, tap to review the username & password. (There is no one location in Android phones to access all passwords.)
- Or open the specific app, then settings > user account, to learn the email account used to set it up. Use this email address to log into the corresponding cloud service ( Carelink, Clarity, Libreview, OneTouchReveal etc). Click "forgot password" to reset it if can't recall. The email used to set up the app must be used to sign into the online cloud service. Connect with the company IT or rep for help if needed.
- Additionally, although not ideal for the depth of data, a screenshot can be taken and emailed to a clinician.
Apps for "Bolus Calculators" or "Insulin on Board". We cannot endorse the accuracy of these apps.
- Ypsomed App: This app is intended to pair with the Ypsomed pump, but the option exists to choose MDI and see Insulin on Board.
- Lifescan Insulin Mentor has a bolus calculator that can be used independently from their meters, if desired. See the meters page and use <Ctrl + f> to search for ‘Mentor’.
See Carbohydrate Counting Heading below for related apps.
Assessment Tools and Safety
See the Diabetes Canada Quick Reference Guide for a short summary of screening, targets, glycemic therapies, cardiovascular protection, preventing hypoglycemia and goal seting. See this resource for Time Management guidelines.
- Assess Diabetes Risk/Screening:
- Assess Agenda:
- Click to view Client Centred Counseling: Interview Overview below
- Agenda setting webpage
- Assess Safety:
- Diabetes safety checklist (psych-social, hypo, hyper, DKA, HHS, DIP, vascular, wounds)
- Psychosocial Patient health questionnaire (PHQ)
- Assess Targets and Complications:
- See our Diabetes Targets and Priorities page
- Assess if vascular protection medication required- See Diabetes Canada Interactive Tools
- Diabetes care flow sheet and targets (Diabetes Canada)
- Assess Patient Knowledge:
- If problems opening PDFs, right click, "save as", save to your desktop.
- Carbohydrate Counting Quiz 2026 - pdf, AHS
- MDI patient knowledge quiz (ICR, ISF, managing DKA, hypo)- pdf, AHS
- Managing Your Blood Sugars Worksheet -pdf, AHS
- Pump Annual Review: IPTP Self Assessment Questionnaire - pdf, AHS
- Pump: DKA Prevention in Pump - Practice Cases for Patient- pdf, AHS
- Pump: Intro to Pump Patient Questionnaire -pdf, AHS
Biosimilars
A biosimilar insulin is highly similar to another insulin (with an expired patent). No differences in clinical performance are expected from the biosimilar in comparison to the original medication. Government drug plans, such as those in Alberta, often promote the use of biosimilars as they are frequently lower in cost. For use of biosimilar insulins in insulin pump brands, see here.
Blood Glucose Logs & Records - click to redirect
Carbohydrate Counting
The following are some of the many tools available for determining the carbohydrate content of foods. Not all sources of carbohyrate content may be acccurate (particularly for apps). For suggested nutrient intakes in diabetes, see Diabetes Canada Guidelines Chapter 11 - Nutrition Therapy.
Carb Counting Handouts
- Healthy Meal Planning for Diabetes (lists 15g carb choices). See the NFS Online Database in Nutrition Resources below. (AHS)
- Matching Insulin to Carbohydrates Handout under Diabetes -Type 1 heading below. (AHS-DCC)
- Basic Carbohydrate Counting (Diabetes Canada)
Other Carb Info and Resources
- Labels: Subtract grams of fibre from the grams of carbohydrate for the portion on the label.
- Restaurant websites: Many fast food and other restaurants have nutrient analysis posted online for their products.
- Diabetes Canada Educator Resource: Helpful hints for educators using Beyond the Basics
- Ordering Beyond the Basics
- Nutrient Analysis Apps: Through smart phones' app stores or AppCrawlr .
- General carbohydrate estimates. One carbohydrate choice contains 15 grams of carbohydrate (after the fibre is subtracted).A general guideline for the number of carbohydrate choices to eat per meal is 2-4 for most women and 4-6 for most men. For snacks: 0-1 for women and 0-2 carb choices for men.
One Carb Choice (15g) equals:- 1 slice of bread
- 1/2 cup (125 mL) cooked pasta/potato/other starch
- 1 medium piece of fruit
- 1 cup (250 mL) of milk
- 1 tbsp (15 mL) of sugar, jam or honey.
Nutrient Analysis Websites or Apps
We cannot verify accuracy of data. Some apps or websites have customers input data. Please advise patients to carefully consider options and pricing. The product manufacturer or label is always the best resource for processed foods.
- Canadian Nutrient File
- MyFitnessPal Recipe Calculator
- MyNetDiary
- Self Nutrition Data
- Calorie King
- Sushi nutrient analysis
- Canadian Nutrient File (downloadable file)
- USDA Nutrient Database (online use)
- SNAQ-Food & Glucose Record
Classes for Diabetes (for patients)
- Alberta Healthy Living Program
AHLP classes, offered virtually, can be booked on-line at Alberta Healthy Living Program. Search classes by topic (i.e. diabetes) rather than by zone. - Diabetes Canada Type 2 Live Virtual Classes
Diabetes Canada Type 2 Virtual Classes as well as their toll-free phone & email support. - Diabetes Canada Type 1 Video Education Series
- Primary Care Networks (PCNs)
Encourage patients to contact their Primary Care Network (PCN) regarding classes. PCN information can be accessed through mypcn.ca - Okaki Diabetes Virtual Care Clinic for Indigenous People in Alberta
“OKAKI’s Diabetes Virtual Care Clinic (ODVCC) This service is for any self-identifying Indigenous person or family member and any person living in or working in or around a First Nation or Metis settlement in Alberta with a diagnosis of pre-diabetes or diabetes. The ODVCC consists of diabetes specialists, certified diabetes educators and other allied health professionals. Those interested in services or online classes to call 587-882-4477. Clients can self-refer to the group classes by emailing . Physician referrals are here. - Also see Diabetes Prevention
Client Centered Counseling (Motivational Interviewing)
- Diabetes Canada
- A handy guide to motivational interviewing
- Decisional Balance Tool for those with low conviction.
- Our resources:
- Other
- Read: Tips for Instructing Groups
- Read: 3 Minute Empowerment - Dr. Jacques Bedard
- Read: Motivational Interviewing in the Prevention and Management of Chronic Disease: Improving Physical Activity and Exercise in Line with Choice Theory.International Journal of Reality Therapy, 2008: 27(2):26-29.
- Read: Welch G, Rose G, Ernst D. Motivational Interviewing and Diabetes: What Is It, How Is It Used, and Does It Work? Diabetes Spectrum January 2006 Vol 19 (1): 5-11
- Visit and browse your PCN Learning Resources (ABSORB) for courses
- Visit and browse My Learning Link for AHS staff for courses
Complications
- See heading for Assessment Tools and Safety above
- Staying Healthy with Diabetes - Diabetes Canada handout
- See our Complicatons page
Computer and Internet Access for Patients
Some patients do not have access to a computer and/or internet or do not have adequate skills to help them navigate online. Unfortunately, they cannot benefit from servers that upload glucose or other data into reports or even from haing an email account. Please note the possible resources to help these patients.
- All Calgary Public Library (CPL) locations (except for Rocky Ridge) have computers with internet access and printers available for members to use.
- These computers don’t need to be booked. People need either a Calgary Public Library card (free if live in the city; can sign up by calling 403-260-2600 or in-person) or to connect with a staff member to get a guest internet-only card.
- CPL regularly has introductory technology programs. These can be booked online or by calling the library. Details are here. Usually these sessions are in person with safety measures per local COVID protocols.
- CPL has a volunteer-led program called Tech Mentors which assists members one-on-one with specific inquiries (e.g. setting up a gmail account) or assists members who need more individual help. This help is available either online or in person (but not at all sites, so members need to call to ask.)
- The Alex may have computer access, although it may be discontinued during COVID. Patients can call to ask 403-520-2260.
Continuous Glucose Monitors (CGM)
- Targets for CGM (% TIR, TBR, TAR. See the relevant link in Diabetes Targets, A1c and Glucose Levels here.
- How to analyze CGM data
- Handouts
- Continuous Glucose Monitoring (CGM): The Basics (AHS)
- Glucose Sensors: Suggested Practices
- Dexcom Trend Arrows: Preventing High & Low Readings by Adjusting
- Libre Arrows: Scanning Frequency & Adjusting Insulin Using Trend Arrows
- Related pages:
- Cost Coverage Heading on this page, just scroll.
- Dexcom Clarity cloud server at https://clarity.dexcom.eu/
- LibreView cloud server
- Medtronic Guardian Connect CareLink cloud server
- CGM Brand Information page - for company contacts and more
- Skin Care Products
- Continuous Glucose Monitoring Home page.
- Benefits and Challenges of CGM
Cost Coverage Information (Alberta)
Patients are encouraged to meet with psychosocial services in their PCN or diabetes centre to review potential additional options available to help assist with the costs of managing diabetes. If there is nothing specific listed further down, patients could also consider approaching alternate groups such as:
- Lions/Lioness Clubs
- Royal Purple organization
- Legions
- Larger companies/business as sometime either the business or employees may have funds they collect for community types of goodwill funding
- Churches
See the Psychosocial page for financial resources available in Alberta
Diabetes Canada Resources
- Diabetes Canada Interactive Tools
- Clinical Practice Guidelines - online version
- Appendices: Diabetes Canada Flowsheets etc
- Managing type 2 diabetes during COVID-19: a guide for primary care providers
- Diabetes Education Line or 1-800-BANTING where a volunteer certified diabetes educator provides individualized answers and support.
- Webinars for those with diabetes
- Virtual diabetes education classes for those with type 2 diabetes.
Diabetes in Pregnancy
Calgary DIP Clinics, referral and fax numbers see here, and scroll down to Diabetes in Pregnancy.
COVID-19 and Pregnancy
General Pregnancy Resources:
- Antenatal resources for healthcare providers (updated July 2019): Alberta Antenatal Pathway
- Resource provided to patients by their primary care team when pregnant or planning pregnancy: Healthy Parents, Healthy Children (healthy weight gain, exercise, etc.)
- Best Beginning Program:
- Best Beginning - Referral Form
- Best Beginning - Birth and Babies
- Best Beginning - Alberta Referral Directory
- Nutrition Guidelines for Pregnancy (Nutrition Services) - (see diabetes specific guidelines below)
Gestational Diabetes (GDM) Resources:
- Patient Video: Gestational Diabetes - How to manage with healthy eating and activity(DCC)
- Patient Video: Starting Insulin in Diabetes in Pregnancy (DCC)
- Patient Handout: Gestational Diabetes (Diabetes Canada)
- Patient Handout: After Gestational Diabetes (Diabetes Canada)
- Patient Handout: Metformin Use in GDM
- Fillable Food Record
- Fillable Blood Sugar Log with comments
- Fillable Blood Sugar Log with medications
Diabetes in Pregnancy: Other Resources
- Diabetes Canada Guidelines, see chapter on Diabetes and Pregnancy
- DCC Pre-Existing Diabetes in Pregnancy Webpage
- DCC Gestational Diabetes Webpage
- Diabetes Safety Checklist - choose pregnancy
- Patient-facing Diabetes in Pregnancy Webpage for appt prep
- External website resource for patients with GDM, type 1 or type 2 diabetes in pregnancy: diabetes-pregnancy.ca
- Nutrition Guidelines for Diabetes in Pregnancy (Nutrition Services- updated 2018)
- Forum for Injection Technique (FIT): Guidelines for insulin injection in pregnancy.
- Patient Handout:Pregnancy and Type 1 or Type 2 Diabetes
- Patient Handout:Type 1 and type 2 diabetes After Pregnancy
- Nutrition handouts for diabetes in pregnancy see
Diabetes Prevention
- AHS Virtual Diabetes Prevention Program:
Clinicians, please email to learn how to enroll your patients for the AHS virtual Diabetes Prevention Program (https://www.albertahealthservices.ca/scns/Page13961.aspx )”
Diabetes Services (AHS) & Referrals - Calgary Zone
Diabetes -Type 1
- Education:
- Diabetes Canada Type 1 Video Education Series ("How to Type 1")
- Type 1 diabetes: the basics - one small PDF download (Diabetes Canada)
- Type 1 Diabetes Education Full Review (Large PDF download)
- Basic nutrition guidelines for type 1 diabetes (AHS)
- Activity and type 1 diabetes (AHS)
- How to Manage Illness in Type 1 Diabetes and Prevent Diabetic
Ketoacidosis (DKA - Matching carbohydrate to insulin (and using ISF - correction factors) - patient handout
- Low blood sugar: go to heading Hypoglycemia
- Diabetes and Driving (AHS)
- To search AHS Nutrition Database for handouts, see Nutrition Resources below.
- See Glucose Meters heading for logbooks and blank record books.
- See Lipohypertrophy webpage
- See Glucagon Heading
Diabetes-Type 2
- Type 2 Diabetes - The Basics (Diabetes Canada Handout)
- Search this page or Diabetes Canada's patient resources for more handouts
Diabetes Updates
- Sign up for periodic emails reivewing new meds, gadgets, etc in diabetes (for heathcare providers)
- View archives
Donating Supplies
- General Diabetes Supplies
- Pumps & Pump Supplies:
- JDRF (1.877.287.3533, ) or Diabetes Canada (1-800-226-8464, ) may know where to donate pumps and supplies. Please consider asking them.
- The Calgary Insulin Pumpers group (contact page is here) may accept them as their members may not all have insurance or Alberta Insulin Pump Therapy Program coverage.
- Richmond Square Pharmacy in Calgary may accept unused pump supplies. (403) 249-4346
- Medtronic pumps: Medtronic may help someone donate a Medtronic pump to someone they specifically know. It's possible the person receiving the pump pays $500 to have the warranty transferred. Medtronic takes the pump back and provides a new one. If this is someone in Alberta, it is preferred for them to go through the Alberta Insulin Pump Therapy Program (IPTP) for funding of supplies and pump.
- Insulin for LIfe no longer has their donation service.
- CUPS primary care clinic will accept diabetes supplies and unused insulin that has not expired. Supplies can be brought to the CUPS clinic. Please call first (403-221-8780 dial 1 to talk with primary care clinic) and they will instruct re: drop off.
Driving
- Patient Handout: Diabetes and Driving (AHS)
- Patient Handout: Drive Safe with Diabetes (Diabetes Canada)
- Diabetes Canada Guidelines Chapter on Driving
- Note that Physicians adhere to the CCMTA Drivers Medical Standards [Canadian Council of Motor Transport Administrators]. Any questions about interpretation should be directed to the CCMTA and the Alberta Ministry of Transportation. People using insulin will be required to submit a Medical Examination for Motor Vehicle Operators.
Emergency Wait Room Times
Endocrinology & Metabolism Patient Services
- Visit our Ucalgary Patient Website at www.endometab.ca for all Endocrinology & Metabolism Program, Calgary services as well as patient resources
- Or view just our diabetes services
Exercise
- See heading for Physical Activity
Foot Care
Health Care Provider Foot Care Assessments and Resources
- Also see our Foot Care webpage
- The Diabetes Foot Health Self-Screening Tool: This tool has been developed to support patients in screening their feet at home, identify their overall risk of developing foot problems, and the actions to take depending on the risk level.
- Why a Proper Foot Assessment is Important- DON SCN Video
- Specialist Link Diabetes Foot Care Primary Care Pathway (One pager!)
- Foot Care Pathway: Alberta Diabetes Foot Care Clinical Pathway (DON SCN) Assessment Tools and Resources
- Additional reading: The American Podiatric Association's Guidelines
- Monofilaments - Reusable (with cleaning, appropriate for use on multiple patients):
- PediCare Professional Foot Care Instruments (search: filament)
- Health Care Solutions (search: filament)
- Monofilaments - Disposable (not for use on more than one patient):
- AutoControl Canada (search: filament)
- PediCare Professional Foot Care Instruments (search: filament)
- Wounds Canada
- Note, some clinics give a disposable monofilament to the patient directing him/her to bring it back to appointments for reuse at future foot checks.
Footcare Handouts and Patient Resources
- Encourage patients to ask their PCN about services. e.g. Mosaic PCN offers those living in their catchment area classes and individual appointments for foot care.
- Alberta Aids to Daily Living may provide therapeutic footwear or orthotics for those who qualify and who are prescribed this by a physician in one of Alberta's High Risk Foot Teams. In Calgary the clinic that can prescribe is the Zivot Limb Preservation Centre at PLC.
- DON SCN Alberta Foot Care Patient Handouts & Online Education
(Contact if you would like to request a staff presentation on the Diabetes Foot Care Clinical Pathway)
- Diabetes Canada Patient Handouts:
Calgary Foot Care Services: Low - Moderate Risk
- Alberta Foot Care (previously Victoria Order of Nurses)
- College of Podiatric Physicians of Alberta website to find a current list of podiatrists and clinics in Calgary.
- Kerby Centre for Seniors Foot Clinics
- If finances are a concern, suggest patients call local podiatry services and ask what is charged for initial assessement and ongoing footcare appointments.
Calgary Foot Care Services: High Risk
If patient has a wound refer to the Sheldon Chumir wound clinic.
- The Sheldon Chumir Wound Clinic information.
Fax Referrals to Community Care Access 403-943-1602
Fax both the Foot Risk Assessment Form together with the Wound Clinic referral form. - Peter Lougheed Centre: Zivot Limb Preservation Centre information.
- Fax number: 403-943-6423.
- Fax both the Foot Risk Assessment Form together with the PLC referral form.
- IMPORTANT: Educators MUST include the name and info of the MD who referred to DCC (GP or Endo). Zivot will send the report back to that physician. You can include your name in the signature as an educator from Diabetes Centre Calgary and add "for Dr. ...(referring doctor)." As per usual charting standards, please inform the referring physician of the action you've taken.
Fructosamine
- Serum fructosamine may be used as an alternative to Hemoglobin A1c. It indicates average glucose level over the previous 2-3 weeks.
- According to Medscape (https://emedicine.medscape.com/article/2089070-overview#showall) updated October 2019, the formula for comparing HbA1c to fructosamine is:
- HbA1c = 0.017 X fructosamine level (µmol/L) + 1.61
- Detailed infomation on serum fructosamine available in this review by Dr. Ghaznavi and Dr. McKeen.
Gastroparesis
- If you suspect your patient may have gastroparesis, you can advise they discuss with their endocrinologist or primary care physician.
- A patient handout is available on the AHS Nutrition Education handouts page here. Use the search box to search "gastroparesis". Refer to a dietitian.
- Physicians can consult Specialist Link with patient related gastroenterology questions.
- CMAJ Gastroparesis (quick summary). Refer patients to physicians for discussion of any medications.
Glucagon
- See the Complete Medications Table for Baqsimi handout and video).
- Glucagon and diabetes handout (AHS). Older as discusses injections.
Glucose Management Indicator (GMI) for CGM
- Simply put, GMI replaces the terms "Estimated A1c"and 'eA1c' that were used in glucose sensor reports. Eventually eA1c will be removed from most sensor reports. GMI estimates the A1c using average sensor glucose data of ideally ≥ 14 days. GMI may be reported in % or mmol/mol (as is A1c).
- GMI and A1c are not the same and may differ for various reasons including individual’s biology or a short-term fluctuation in glucose control.
- Convert GMI mmol/mol to GMI% (A1c conversion chart)
- Convert average sensor glucose to GMI% (Calculator)
- For GMI use in Medtronic reports, see here.
Glucose Meters
- Accuracy of blood glucose meters
- Glucose Meter Summary Sheet for Health Educators 2021 (Includes steps to manually access results etc)
- CGM- See CGM Heading for continuous glucose monitoring
- Cloud accounts and clinic upload boxes
- Diasend portal . The Diasend Professional Clinic box will upload Libre handheld scanners, glucose meters, most CGM cloud server data, most insulin pumps (Omnipod, Tandem, Ypsomed) and merge glucose and pump data. See the Diasend document: Interpretting Charts and Graphs.
- Glooko portal to access professional & personal accounts. (The clinic Glooko box currently doesn't upload Libre - Oct 2019.)
- In many cases, patient data is accessible via company specific cloud services or apps. See specific meter brand websites listed on Glucose Meters page or CGM Brands page. e.g Libre phone app users can view their data by signing into their cloud account on Libreview, Dexcom on Clarity.
- Diabetes Canada Interactive Tools for glucose monitoring frequency
- Glucose Meters page. Also includes link to the Genteel lancing device.
- Health Canada: Approved medical devices.
- Patient Handout: Managing your blood glucose (testing blood sugar, sick days (Diabetes Canada)
- DOWNLOADABLE LOGBOOKS / RECORD SHEETS
- 4 Day Food, Insulin and Blood Sugar Worksheet (AHS)
- Fillable food and glucose record sheet
- Your Blood Sugar Log Fillable PDF Versions:
- English: Your blood sugar log-Fillable PDF (AHS)
- French: Your blood sugar log-Fillable PDF (AHS)
- Spanish: Your blood sugar log-Fillable PDF (AHS)
- Arabic: Your blood sugar log-Fillable PDF (AHS)
- Urdu: Your blood sugar log-Fillable PDF (AHS)
- Tigrinya: Your blood sugar log - Fillable PDF (AHS)
- Traditional Chinese: Your blood sugar log - Fillable PDF (AHS)
- Vietnamese: Your blood sugar log-Fillable PDF (AHS
- Blank glucose record book (AHS)
- Glucose Log Book (Diabetes Canada)
- Pump records: 5 days: Glucose & insulin records for pump and 3 days: Blood glucose and insulin record for pump therapy
HbA1c - Hemoglobin A1c
- Patient handout: A1c Testing for Adults - handout (AHS)
- Visit our A1c page for why A1c matters (research summaries) and what A1c is
- Diabetes Canada Interactive Tool - Individualizing A1c
- Video: Diabetes Canada's What, When, Why? Understanding A1c
- Glucose Wands (Canadian Orders, see page 72) or (U.S. orders).
Healthcare Provider Education
Homecare
- Calgary area clients and staff may call 403-943-1920 to inquire about eligibility for homecare services.
- Homecare staff are not permitted to take insuiln orders or adjustments from educators. DCC educators please refer to their Medication Adjustment Policy for options (e.g. if familiy is adjusting instead, a certain consent is required).
Hypoglycemia (Low Blood Sugar)
- Diabetes Canada Handout: Hypoglycemia or Low Blood Sugar
- Patient PICTORIAL handouts:
- Low Blood Sugar (AHS) English
- Low Blood Sugar (AHS) Tigrinya
- Low Blood Sugar (AHS) Arabic
- Low Blood Sugar (AHS) French
- Low Blood Sugar (AHS) Spanish
- Hypoglycemia in Adults (Diabetes Canada)
- Patient handout: Hypoglycemia unawareness: When you don't feel your low blood sugar (AHS)
- Patient handout: Glucagon and diabetes (AHS)
- Educator references:
Indigenous Health Services
- Indigenous Support Line: 1-844-944-4744: Support for issues related to referrals, culture, primary care, addictions mental health, and other general concerns. Poster is available here.
- NIHB (Non-Insured Health Benefits Program): Libre and Dexcom sensors are covered under NIHB. Patients to connect with their pharmacists once they have a prescription.
Inpatient & Outpatient Diabetes Resources & Supporting Documents (Alberta Health Services)
- AHS Clinical Policies & Procedures page is searchable. Click here.
- AHS Clinical Knowledge Topic Viewer - under "D" for diabetes. e.g. for DKA treatment and under "P" for Perioperative Management of Patients with Diabetes
- Provincial Diabetes Medication Adjustment Protocol (Adults) - e.g. AHS adjustment protocol for AHS educators
- Provincial Inpatient AHS Glycemic Policy: Glycemic Management Policy Suite (includes inpatient Hypoglycemia and Hyperglycemia Policies)
- Provincial in-hosptial insulin pump guidelines at www.ipumpit.ca
- Provincial AHS Insulin Safety & Diabetes Management for Health Care Professionals includes:
- General Diabetes Information
- Nutrition Information for Patients with Diabetes
- Basal Bolus Insulin Therapy (BBIT)
- Insulin Pump Therapy (IPT) – Safe Management in Acute Care
- Provincial Glycemic Management Policy Suite
- General Information on Insulin Safety
- Insulin Pen Information
- AHS Insulin Formulary Information
- Provincial: myLearningLink > Courses and Registration>Basic Diabetes Education - this is designed for inpatient staff.
- Provincial BBIT
- Basal Bolus Insulin Therapy (BBIT) in Hospital Self Study Guide (AHS - Provincial)
- Basal Bolus Insulin Therapy (BBIT): AHS educational materials for professionals
- Insulin Pump Therapy In Hospital: AHS processes and documents
- Provincial: Checking your blood glucose (sugar) level while you’re in the hospital
- BD AutoShield Duo Safety Pen Needle Video
- Calgary Zone Inpatient Diabetes Nurse Navigator: Click here for summary sheet of our role.
- Diabetes Services Search Engines, when referring to AB Clinics:
- Edmonton Zone Diabetes Services 780-735-2824 referral is here. Visit their site for referral criteria here.
- Inpatient foot care options: Inpatient units may consult geriatric untis (e.g. Units 57 & 58 Acute Geriatrics at RGH) to learn their local practices for inpatient nail/foot care. Different options may be used in the province, some including long term stay clinics contracting a foot care nurse whereas others inviting families to hire a private foot care nurse. General resources: www.ahs.ca/footcare and https://www.albertapodiatry.com/
Insulin Adjustment
- Please see related headings on this page:
Insulin Allergy
Insulin allergies were more common with bovine and porcine insulins. As technology has improved with recombinant and analogue insulins, the reported prevalence of insulin allergy is 0.1-0.3%.
If your patient lets you know about a reaction to their insulin, it is important to gather appropriate history and inform the patient’s family physician or diabetes specialist. Assessment considerations:
- Type of reaction? *A diffuse, systemic response requires prompt assessment and treatment*
-local (immediately around injection site) or diffuse (covering large area of body)?
-skin only, or systemic (airway/breathing)?
-Does it resolve, or worsen over time? - Relationship to insulin administration?
-immediately -1 hour after injection
-delayed- 2-24 hours after injection - Type of insulin?
- Changes or interruptions to insulin?
- History of other allergies? (many needles use silicon or lubricants)
- Any other triggers such as change to medications, diet, cosmetics, detergents or other autoimmune diseases?
Treatment considerations to be discussed with physician or diabetes specialist, depending on severity of reaction:
- Observe and optimize patient’s injection technique to avoid any possible site irritations (i.e. proper site rotation, not injecting where clothes/belts rub, not massaging after injection, not using alcohol wipes)
- Cool site before and after injection
- Possible use of insulin port devices if allergy to pen needles
- Avoid insulin if possible
- Switch to a different type or brand of insulin
- Use of anti-histamines for symptom relief
- Rapid desensitization protocol – complex protocol that involves starting insulin at very low doses in an intensive care setting
Insulin Pump
- Alberta Health Services Insulin Pump Resources
- Alberta Health: Alberta Insulin PumpTherapy (IPT) Program Site
- AHS Approved Specialist Physicians for Alberta IPT program - see endometab.ca > Refer (and scroll down to insulin pump)
- Insulin Pump Therapy Patient Learning Module for Patients (online) and accompanying questionnaire.
- Guidelines for safe management of insulin pump therapy in hospital (AHS)
- Troubleshooting Hypo and Hyperglycemia in insulin pump therapy
- Skin care products for infusion site management
- Patient Handouts & Forms:
- See the "Assess" Heading (click here) for Assessment Quizzes (DKA, MDI, Carb)
- Basal testing worksheet- Checking and adjusting basal rates in insulin pump therapy (AHS)
- Coming off pump (AHS)Coming off pump (AHS)
- DKA- Prevention of Diabetic Ketoacidosis (DKA) in Insulin Pump Therapy for Adults(AHS)
- DKA prevention in insulin pump: Practice Cases (pdf)
- Emergency / Urgent Care Insulin Pump Document
- IPTP Patient Responsibility Agreement
- PATIENT INFORMATION- INSULIN PUMP PROGRAM - DIABETES CENTRE CALGARY
- Records: Blank pump glucose/insulin records
- Hands on Information Nights at Carriage House Inn in Calgary, second Tuesday of each month.
- Support Group: Calgary Insulin Pumpers
- Other: Comparison of AID pump systems Canadian and a US site (please note this PANTHER Program® is currently funded by grants from the Helmsley Charitable Trust and Tandem Diabetes Carplease note this PANTHER Program® is currently funded by grants from the Helmsley Charitable Trust and Tandem Diabetes Care: Comparison of Automated Insulin Delivery US devices (pumps)
- Other: Commentary on Automated Insulin Delivery: Six Universal Observations and Understandings
Insulin Review
Periodically, consider reviewing the following with those using insulin. In practice, glucose levels are frequently impacted by one or more of the following. Perhaps consider an annual "Insulin Review" with patients to touch base on:
- role of insulin
- type and action(s) of insulin(s) prescribed and carbohydrate requirements
- use of insulin delivery device and accessories
- time that insulin is administered (e.g. before or after meals etc)
- storage (in the fridge, no freezing) and expiry of insulin (see Complete Medication Table for duration at room temperature)
- injection sites and rotation
- pen needle length (e.g. not 12 mm, to avoid intramuscular injections)
- barriers to giving all injections, if any
- impact of missed or late injections
- driving
- travel (e.g. 2x supply in carry-on)
- basics of how and when to self-adjust bolus and basal insulin if appropriate (use of ICR and ISF; targets used with ISF)
- when and how to seek help (Consider giving the handout: Diabetes Resources for Patients. It contains a list of urgent concerns.)
- hypoglycemia (prevention, symptoms, treatment)
- hyperglycemia/DKA (prevention - ketone testing, symptoms, treatment)
Insulin Safety - AHS Provincial
Insulin Senstivity Factor (ISF)
Insulin Starts and Injectables
- DCC staff: print Medication Supply Checklist to provide patient
- Diabetes Canada Resources
- Getting started with insulin handout;
- Insulin Pen Start Checklist for Healthcare Professionals
- Traditional Chinese: Getting started with insulin (handout)
- Video: How to Inject Insulin Step by Step Guide length 7m:39s
- Video: Insulin Pen, What You Need to Know length 2m:22s
- Video: Introduction to Insulin length 2m:45s
- Alberta Health Services (AHS) Resources
- Forum for Injection Technique (FIT)
- For more detailed information on insulin visit the Complete Medication Table.
Knowledge Resource Services (KRS - AHS "Library")
Marijuana (Cannabis) and Diabetes
- Impact of Marijuana use on Diabetes Management:
- Marijuana may also indirectly impact diabetes management through its negative effects on self-care practices, decision making, appetite, judgement, memory or other effects.
- Review Diabetes Canada Position Statement on Recreational Cannabis Use in Adults and Adolescents With Type 1 and Type 2 Diabetes (2019)
- For more information visit:
Medical Procedures
Generalized Summary: (scroll a few inches for more options for pump)
- Basal Insulin:
20% reduction in basal insulin the night before and morning of a procedure. Tresiba (degludec) may need to be reduced 2-3 days prior. (No reduction is suggested for fasting labwork unless individually required for safety.) - Bolus Insulin:
The day(s) of clear fluid preparation, consider reducing meal bolus by 20%.
The morning of the procedure, hold bolus insulin until eating after the procedure.
For hydrogen breath test for small intestine bacterial overgrowth, consider reducing the bolus by 20% for the75g glucose required for the test. - Meds other than insulin:
- Consider holding SGLT-2 two days before colonoscopy prep to reduce the risk of DKA.
- The morning of the GI procedure, hold other diabetes meds until the patient is eating after the procedure.
- GLP-1 & Dual GLP-1/GIP Receptor Agonists: No change in dosing is required for GI tests including colonoscopy. Advise the patient to discuss potential extended preparation with their GI team. For procedures requiring general anesthesia, advise the patient to discuss GLP-1 & Dual GLP-1/GIP Receptor Agonists dosing with their surgical team.
- Individualization and more:
These suggestions need to be individualized according to the patient's current glucose values, risk for hypoglycemia and other factors. See handouts below for additional instructions for specific tests.
Patient Education for Medical Procedures (AHS myHealthAB):
- Adjusting Your Diabetes Medicine & Diet for Fasting Blood Tests
- Adjusting Your Diabetes Medicine & Diet for a Hydrogen Breath Test (HBT) for Lactose intolerance
- Adjusting Your Diabetes Medicine & Diet for a Hydrogen Breath Test (HBT) for Small Bowel Overgrowth
- Adjusting Your Diabetes Medicine & Diet for a Gastroscopy or EGD
- Adjusting Your Diabetes Medicine & Diet for a Barium Enema or Colonoscopy
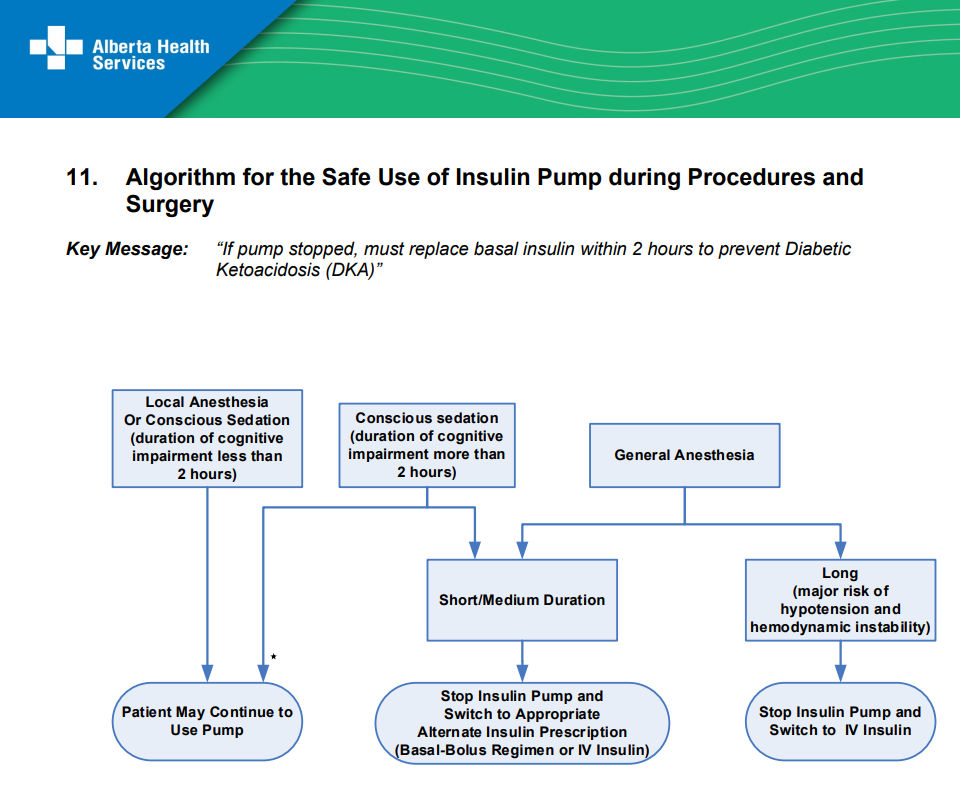
Algorithm for the Safe Use of Insulin Pump during Procedures and Surgery
There are resources for the safe use of insulin pump therapy in hospital. Some of these guidelines may also apply to outpatient procedures requiring local anesthesia or conscious sedation, in particular this resource: Algorithm for the Safe Use of Insulin Pump during Procedures and Surgery. Alternately, click the image below to enlarge.
For patients that come off pump for procedures and have insulin replaced by IV or manual BBIT, please instruct on how to safely resume basal insulin in pump and automated delivery of correction or basal insulin if being used (AutoMode, Control IQ, Loop, APS etc). This will vary depending on how insulin was replaced when the pump was removed, how much of that replacement will still be active and for how long.
Medication Resources
- AHS Clinical Polices and Procedures (here)
- Adjustment Guidelines & Next Line Agents
- Complete Medication Table.
- Cost Coverage information: See Psychosocial Resources
- Health Canada Drug Product Database for product monographs
- Inpatient Providers: See Inpatient Diabetes Resources heading aboveInpatient Providers: See Inpatient Diabetes Resources heading above
- Intro to Diabetes Medications (our webpage)
- Renal Impairment: Diabetes Canada - Antihyperglycemic Agents & Kidney function
- Renal Impariment: See Renal Disease heading below.
- Patient Medication Handouts (LexiDrug & Diabetes Canada)
- Safety
- See Hypoglycemia Heading above
- PADIS - Poison and Drug Information Service 1-800-332-1414
- SADMANS Sick Day Medication List (Diabetes Canada)
- www.drugcocktails.ca - Enter a prescription medication (ie. Insulin) and any interactions with alcohol, illicit drugs, tobacco or marijuana will be listed.
Nutrition Resources
- Alberta Health Services Nutrition and Food Services (AHS NFS).
- Nutrition guidelines for all clinicians are available at AHS Nutrition Guidelines for Healthcare Providers .
- More detailed guidelines are available to RDs within AHS on the Nutrition Services Hub > Guidelines & Practice Support Tools.
- Publicly Available AHS Nutrition Education Materials (Click on Diabetes).
- Calgary: Access to Food Resources
- Canada's Food Guide (Health Canada)
- Diabetes Canada Nutrition Handouts
- From basic guidelines, glycemic index to the ketogenic diet. Use the left-hand navigation bar to search for the resource you need
- Beyond the Basics
- For HCP professional guidelines, see Diabetes Canada Guidelines Chapter 11 - Nutrition Therapy.
- Natural Medicine Database
- PEN: Practice Based Evidence in Nutrition for healthcare professionals.(This link is for access from AHS server computers only). Or visit PEN's home site for subscription information.
Obesity Resources
Physical Activity (Exercise)
- Alberta Healthy Living Program's supervised exercise classes (AHS) Calgary Zone 403-9-Health (403-943-2584)
- Prescription to Get Active (no cost or low cost access to physical activity programs in the community)
- Patient handout: Physical Activity and Type 1 Diabetes
- PCNs
Primary Care Networks (PCNs)
- https://albertafindadoctor.ca/ to find a family doctor.
- Mosaic PCN Diabetes Optimization Team (DOT)
- Patients from Mosaic PCN can refer themselves for an individual diabetes appointment with a Mosaic RD, RN, pharmacist, SW or Behavioral Health Consultant.
Psychosocial Resources
Key Mental Health Resources
- Call 1-833-456-4566 for Canada's Suicide Crisis Hotline
- MENTAL HEALTH HOTLINE 1-877-303-2642. Translation services available.
- Calgary Distress Line: 403-266-4357 (403-266-HELP) Delivers 24-hour support, free crisis counseling and resource referral services to Calgary and the surrounding area.
- Mobile Response Team Call the Calgary Distress Line at 403-266-4357, and ask for Mental Health Crisis Triage. They offer urgent mental health support, assessments and referrals (mobile if necessary).
- Guidelines on how to respond to disclosed Domestic Violence, Abuse or Neglect
See the Psychosocial page for more resources and information
Ramadan
- 2025 Ramadan ended Mar 29.
- 2026 Ramadan starts Feb 17 and goes to to Mar 19
- Diabetes Canada has resources available for patients and educators. Go to www.diabetes.ca and Search for 'Ramadan'
- International Diabetes Federation (IDF): 'Diabetes and Ramadan Practical Guidelines
Research
Renal Disease (Chronic Kidney Disease - CKD)
- Renal Impairment: Diabetes Canada - Antihyperglycemic Agents & Kidney function
- Alberta Chronic Kidney Disease Clinical Pathway
- Alberta Kidney Care Programs
- Jump to
- Diabetes Considerations in Stages 4-5 Renal Disease (DCC older and shorter summary document).
- For Diabetes Centre Calgary staff (interim process):
- Stage 4 (GFR 15 - 30): Check if the nephrologist or endocrinologist is adjusting insulin doses. If not, use the guidelines for Stages 4-5 directly above.
- Stage 5 (GFR <15): If patient is on hemodialysis or peritoneal dialysis, insulin adjustment is the responsibility of the nephrologist or the endocrinologist. Defer to them. For patients on conservative management (no dialysis) insulin adjustment may be done by the nephrologist/endocrinologist, or the educator if that is the preference of the specialist physicians. Use the guidelines above.
Retinopathy
- See our Retinopathy page for information and resources.
- Canadian National Institute for the Blind (CNIB)
Safety Checklist
- See our Diabetes Safety Checklist webpage
Sick Days (Illness)
- Staying Safe with Diabetes When Sick or Dehyrated (Diabetes Canada)
- See heading Diabetes - Type 1 for How to Manage Illness in Type 1 Diabetes & Prevent DKA
- SADMANS Sick Day Medication List (Diabetes Canada)
Skin Care
Smoking Cessation
- Alberta Quits (AHS)
- Your Quit Tobacco Plan - myHealthAB
- Consider directing clients to their family doctor, PCN and pharmacist to ask if they have in-house classes or programs for quitting smoking, and nicotine replacements.
Steroids & Glucorticosteroids (GC)
- See page 29, section 13b. Suggestions for Patients Receiving Corticosteroid Therapy under BBIT.CA > Education & Resources > How to BBIT for Prescribers.
- GENERAL GUIDELINES:
- As the dose of the glucocorticoid is being modified, the dose of
antihyperglycemic needs to be modified - Insulin dose can be adjusted by half the percentage of the GC dose change. For example, when GCs are increased or reduced by 50%, insulin dose is suggested to be increased or reduced by 25%, respectively.
- As the dose of the glucocorticoid is being modified, the dose of
- Prednisone impact on glycemia
- Given in morning, hyperglycemia occurs in afternoon and evening (duration 16-18 hours)
- Peak about 4-8 hours after administration
- Hyperglycemic effect diminishes by morning
- If administered in multiple doses, hyperglycemia may be present throughout the day (mostly post prandial)
- IV hydrocortisone (multiple doses) and Dexamethasone impact on glycemia
- Levels expected to peak about 5 hours after IV administration
- May cause increased glycemic effect through 24 hour period
- May have slight decline in overnight fast
- If patients have blood glucoses equal or greater than 10.0 mmol/L,
- blood glucose lowering therapy should be started.
- Suggested blood glucose lowering therapies: see page 29 of section 13b. Suggestions for Patients Receiving Corticosteroid Therapy under BBIT.CA > Education & Resources > How to BBIT for Prescribers.
- Reduction or Cessation of Steroid
- Reduce insulin or sulfonylurea dose with reduction of steroid dose
- Significant risk of hypoglycemia if insulin dose or sulfonylurea not reduced in line with blood glucose monitoring and anticipated dose tapering
- With once daily steroid especially, there is a high risk of hypoglycemia in the evening,as steroid effect tends to wear off overnight
-
INTERMITTENT DEXAMETHASONE (e.g. 1-2 days/week prior cancer treatment)
- In some cases, glucose does not rise. Assess first, prior to providing extra insulin.
- If required, start with a 10-20% increase of the active insulin* on the dexamethasone days, and potentially one day following. Then resume normal dosing for the remaining 4-5 days.
- Significant monitoring and follow-up is needed to determine individual dosing that works reliably most weeks.
- *Patients on only degludec (Tresiba ) or icodec (Awiqli) are likely to need the addition of bolus insulin.
- Patients receiving D5W on treatment days may need additional insulin. Review the drip rate keeping in mind the following.
- 1000 mL D5W = 50 grams of glucose
- 100 mL D5W = 5 grams of glucose
- X mL of D5W x 0.05 = grams of glucose delivered over the timeframe of the drip (e.g. 600 mL x 0.05 over 2 hrs = 30 grams glucose delivered over 2 hours)
Stress
- See our Psychosocial page for additional information.
- The Diabetes Distress Scale -Diabetes Canada
- Diabetes Canada has several more patient resources available: www.diabetes.ca > Search for "Stress"
- Stress and Your Health - video, AHS
Support Groups & Services
Please note that most of these supportive groups or organizations are not managed, reviewed or endorsed by Alberta Health Services (AHS).
- Alberta Healthy Living Program (AHS) “Better Choices, Better Health" may also involve groups with type 2 diabetes. Click here for offerings.
- Calgary Insulin Pumpers
- Connected in Motion (type 1 diabetes)
- JDRF Southern Alberta - type 1 diabetes
- I Challenge Diabetes
- Roche offers Accu-chek Engage - an online behavioral change support program, for patients who are using the Accu-chek meter. Sign up information is here. Note that patients can register without linking their account to a clinic.
Translated Diabetes Materials (Language, Ethnic/Cultural Resources)
- Search notes:
- Use all of these with caution. They have not been reviewed by Health Canada and do not direct patients to local Canadian resources.
- Important CAUTION: Many of the gestational diabetes handouts available through links below use glucose targets that differ from Diabetes Canada targets. GDM targets are located here and general targets are located here.
- The best way to search for resources is to use"ctrl"+F (pc) or command+F (mac) and type in the language (e.g Punjabi), then hit enter to take you to each listing on this page with that language in its name
- You can also browse the items below
- You may also find possible translated materials under topic headings above e.g. Starting Insulin, Hypoglycemia
- French:
- Diabetes Canada's Ressources Françaises webpage.
- Diabetes Quebec
- Once on website, click EN (English) at the top right of desktop brower. Find the page/handout you want. Then click FR (for French) for the corresponiding French versions.
- Canada's Food Guide
- Tagalog (Filipino):
The Mosaic Primary Care Network and the Filipino Healthcare Providers Group of Calgary provided these handouts. The English resource documents from which these were adapted are in brackets.- Just the Basics - Mahalagang Pamumuhay Para sa Diabetes Tagalog/Filipino (English version is here)
- What is Diabetes - Ano ang Dyabetes Tagalog (English resource doc is here)
- Carbohydrate in Foods Tagalog (no portions included; the English resource doc is here)
- Managing Your Diabetes Tagalog - Paano Manatiling Malusog Kahit may Diabetes (English resource doc is here)
- Driving and Hypoglycemia Tagalog (English version is here)
- Driving Guidelines and Diabetes Tagalog (English version is here)
- Hypoglycemia Tagalog (English version is here)
- Sadmans Tagalog (English version is here)
- Filipino Plate
- Punjabi
- National Diabetes Services Scheme (Australia) has a number of handouts, including for Diabetes in Pregnancy, carb counting, glycemic index and others
- Other
- AHS staff can use Lexicomp (insite>Teams>Pharmacy services>Lexicomp (lower-right):
- Search and select medication or disease condition
- Click desired selection under "Patient Education Results"
- Click on 'English' at top right, and select desired translation
- Click 'Print' to get PDF version.
- www.ethnomed.org: Diabetes information with pictures in a variety of languages (Amharic, Somali, Vietnamese, Khmer, Oromo, Tigrinya, etc.)
- BC Fraser Health Region has a number of diabetes handouts available in various languages, including Arabic, Farsi, Hindi, Punjabi, Tagalog, & Tigrinya
- Seach topic, and select desired language
- Carbohydrate counts of common ethnic foods: Asian, Chinese, Japanese, Indian, Korean, Filipino
- Enhancing Cultural Competency - A Resource Kit for Health Care Professionals (Note that this resource is from 2009 and may contain outdated material. Educators are encouraged to view pages 108 and 109 for the ETHNIC and LEARN models of asking culturally sensitive questions).
- National Diabetes Service Scheme - Australian Government Initiative: (if using any patient handouts please inform patients not to call the contact #'s listed) Many language handouts and videos including resources for Diabetes in Pregnancy. Languages include: Arabic, Bengali, Chinese (simplified and traditional), Dari, Farsi, Greek, Hindi, Italian, Karen, Khmer, Korean, Macadonian, Nepali, Punjabi, Samoan, Sinhalese, Somali, Spanish, Tagalog, Tamil, Thai, Tongan, Turkish, Urdu and Vietnamese.
Travel
- See our Travel page for advice regarding preparation, medication adjustments, and links to patient handouts
- Frio Insulin Cooling Cases may be ordered through their Canadian website.
Vascular Risk
- See Diabetes Canada Health-Care Provider Tools for Reducing Vascular Risk Interactive Tool
- Canadian Cardiovascular Society Resources (apps, pocket guides, guidelines etc)
- Heart and Stroke Foundation of Canada
- Patient handout: Understanding and Managing Your Blood Pressure - Hypertension Canada
- Patient handout: Nutrition and Lifestyle Choices to Manage Blood Pressure
- Hypertension Canada: HCP and patient resources (how to measure blood pressure at home)
- See Nutrition Resources above