It is our responsibilty as diabetes educators to ensure people with diabetes are aware of how to prevent and screen for diabetic retinopathy- the most common cause of legal blindness in people of working age.
1. What is Diabetic Retinopathy?
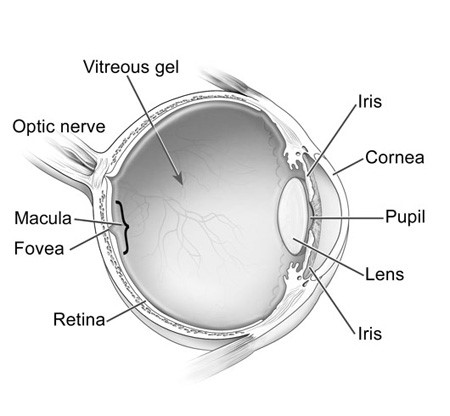
It is important to first understand basic eye anatomy and physiology. The retina lines the back of the eye. Light is focused onto the retina via the cornea, pupil and lens. The light sensitive neurons in the retina convert the light into impulses that are sent through the optic nerve to the brain and interpreted as images. The macula is the central part of the retina, responsible for sharp, straight ahead vision.
Diagram of the Eye
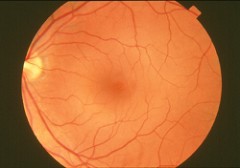
Normal Retina
Diabetic retinopathy consists of three different types- 1) Non-proliferative and proliferative diabetic retinopathy, 2) Diabetic macular edema and 3) Retinal capillary closure.
Non-proliferative and proliferative diabetic retinopathy:
Non-Proliferative (Background) Retinopathy

Non-proliferative diabetic retinopathy is also known as ‘background retinopathy’. High blood sugars can damage the small blood vessels that supply the retina. Damaged blood vessels develop micro aneurysms that leak into eye tissue. These micro aneurysms appear as tiny red dots on retinal images as in picture above.
The swelling blood vessels can cause vessel malformations and blockages leading to poor blood flow to the retina. The poor blood flow triggers growth factors to be released resulting in production of abnormal blood vessels.
Proliferative Retinopathy

Proliferative diabetic retinopathy is distinguished by the presence of abnormal blood vessels. The new blood vessels are fragile and more prone to rupturing and bleeding. Scar tissue develops which can ‘pull’ on the retina leading to increased risk for ‘Retinal Detachment’. Retinal detachment can cause permanent vision loss. The picture above shows the proliferation of blood vessels.
Diabetic Macular Edema:
Example of Distorted Vision with Macular Edema

Diabetic macular edema is swelling of the macula due to damaged and leaking blood vessels. This can happen at any stage of non-proliferative or proliferative diabetic retinopathy. The macula is the central part of the retina, responsible for sharp, straight ahead vision. When the macula is swollen, the central vision becomes blurred and distorted. The above image is an example of how vision may be distorted when macular edema is present.
Retinal Capillary Closure:
Retinal Capillary Closure is a vascular change that can result in blindness and currently has no treatment.
2. How is Diabetic Retinopathy Prevented, Screened for and Treated?
Prevention:
- Glycemic Control: The Diabetes Complications and Control Trial (DCCT), landmark study in type 1 diabetes population, showed that intensive glycemic control (A1c less than 7.0%) reduced retinopathy risk by 76%. Those with some level of retinopathy at the beginning of the study experienced a 54% reduction in progression of retinopathy. Note that the intensively controlled group did experience a transient worsening of retinopathy with overall, long-term benefits. The benefits experienced by the intensively controlled group continued for up to 10 years after completion of the trial as reported in the follow-up study- Epidemiology of Diabetes Interventions and Complications (EDIC). The United Kingdom Prospective Diabetes Study (UKPDS), landmark study in type 2 diabetes population, showed that intensive glycemic control (A1c less than 7.0%) reduced retinopathy risk by 21%.
- Blood Pressure Control: The UKPDS also showed that ‘tight’ blood pressure control (target BP ˂ 150/ 85 mm Hg, actual BP 144/82 mm Hg) lowered progression of retinopathy by 34% and deterioration of vision by 47%.
- Lipids: In type 1 diabetes, dyslipidemia is an independent risk factor for formation of retinal hard exudates and macular edema.
Screening Recommendations:
- Early detection of retinopathy is key to prevention of vision loss. As retinopathy can be present without any symptoms, it is important to reinforce regular eye screening with clients.
- Pregnancy is a risk factor for development and/or worsening of retinopathy in women with type 1 and (theoretically) type 2 diabetes. According to CPG’s, women with pregestational diabetes are advised to have ophthalmological assessment prior to conception, during first trimester, as needed during pregnancy and within the first year postpartum.
- The Clinical Practice Guidelines also recommend the following general screening guidelines:
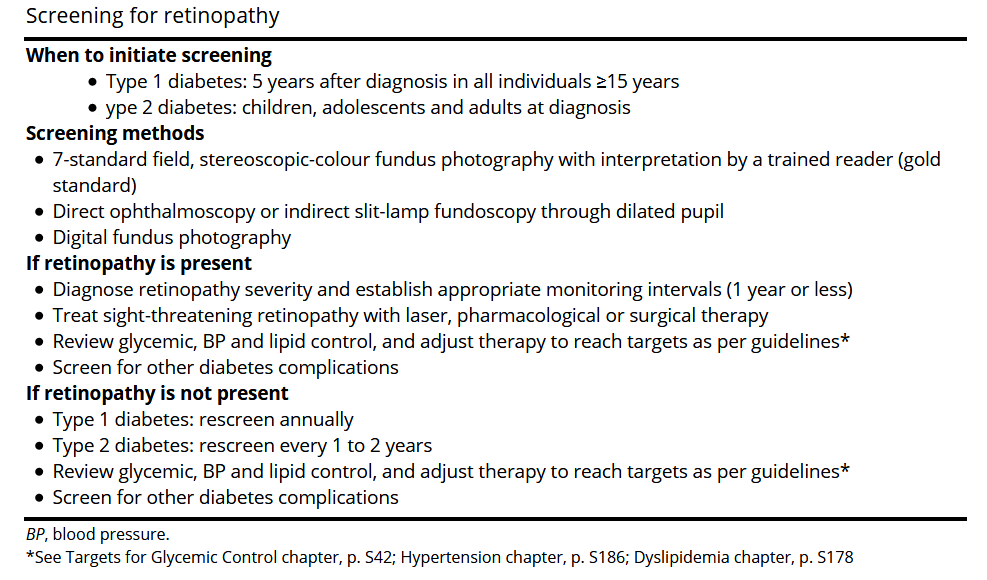
Diabetes Canada Clinical Practice Guidelines Expert Committee. Diabetes Canada 2018 Clinical Practice Guidelines for the Prevention and Management of Diabetes in Canada. Can J Diabetes. 2018;42(Suppl 1):S1-S325. Accessed May 2018.
Treatment:
- Laser Therapy
- Scatter laser or panretinal photocoagulation: Treats severe non-proliferative and proliferative retinopathy by causing multiple tiny laser burns and ‘shrinking’ abnormal vessels.
- Focal laser: Treats macular edema by targeting leaking blood vessels, thereby slowing leakage of fluid and decreasing edema.
- Anti- Vascular Endothelial Growth Factor (VEGF) Intraocular Injection Therapy – treats severe non-proliferative, proliferative retinopathy and macular edema by suppressing the hormone (VEGF) responsible for the formation of weakened, leaking blood vessels. There are two types of injections currently approved for retinal use in Canada – Lucentis (ranibizumab), and Eylea (aflibercept). Avastin (bevacizumab) is not approved by Health Canada for retinal use, however it is often used ‘off-label’ due to reduced cost (CADTH resource).
- Intraocular Anti-inflammatory Injections – Corticosteroid injections alone or in combination with other medications or laser may be used to treat macular edema. Steroid injections have been associated with increased risk for glaucoma so not used as often as other treatments.
- Vitrectomy- Treats severe bleeding into the vitreous by draining the vitreous gel and replacing with saline to maintain eye pressure.
- Fenofibrate medication - Fenofibrate medication in addition to statin therapy was shown to prevent progression of established retinopathy in patients with type 2 diabetes in two trials: Fenofibrate Intervention and Event Lowering in Diabetes (FIELD) and Action to Control Cardiovascular Risk in Diabetes (ACCORD) Eye study.
3. Resources
- Diabetes clients with visual deterioration should be directed to community resources such as the Canadian National Institute for the Blind to acquaint them with technical aids, skill development programs, and relevant counseling services. See topics catalogue for resource links.
- The Freestyle Libre flash glucose monitoring system has 'text to speech' option that can be turned on. See the following excerpt from the Freestyle 'LibreLink' user manual:
- Text to Speech - Turn on Text to Speech to have the glucose reading read aloud when you scan the Sensor. You will hear only your current glucose value and trend arrow direction. Additional information, such as the glucose graph and any message, are available on your My Glucose screen. Remember that Text to Speech inherits the volume settings on your smartphone. If your smartphone volume is turned off, you will not hear the glucose reading read aloud. Tap SAVE when you are done.
- Currently one glucose meter on market with acoustic option- the Oracle Talking Blood Glucose Meter. Go to Glucose Meter page and search 'Oracle' for more information. Note that clients with severe vision loss may have difficulty using lancing device and applying blood to glucose test strip.
- It may help to show clients different glucose meters as they may find some screens easier to read (larger numbers or more contrast).
- Clients may be taught to count ‘clicks’ on insulin pens if they cannot see the number on the dial.
References:
Diabetes Canada Clinical Practice Guidelines Expert Committee. Diabetes Canada 2018 Clinical Practice Guidelines for the Prevention and Management of Diabetes in Canada. Can J Diabetes. 2018;42(Suppl 1):S1-S325. Accessed May 2018.
National Eye Institute: https://nei.nih.gov/
CNIB: http://www.cnib.ca/en/your-eyes/eye-conditions/eye-connect/DR/About/Pages/Overview.aspx