Lipohypertrophy (LH) can impact glycemic control. Studies show various rates of LH in patients from 42%1 to over 64%2. Suboptimal insulin injection technqiues contribute to the development of lipohypertrophy and subsequently the increased risk of variable glucose levels including both hyperglcyemia and unexpected hypoglycemia.
In a worldwide study of over 13,000 patients, routine inspection of injection sites by healthcare professionals was associated with lower A1c levels, less lipohypertrophy and more correct injection site rotation. Yet, only 39% of patients in this study recalled ever having injection sites inspected by a healthcare provider.4 Diabetes educators can perform an important role by regularly reviewing injection sites and techniques.
1. Lipohypertrophy Explained
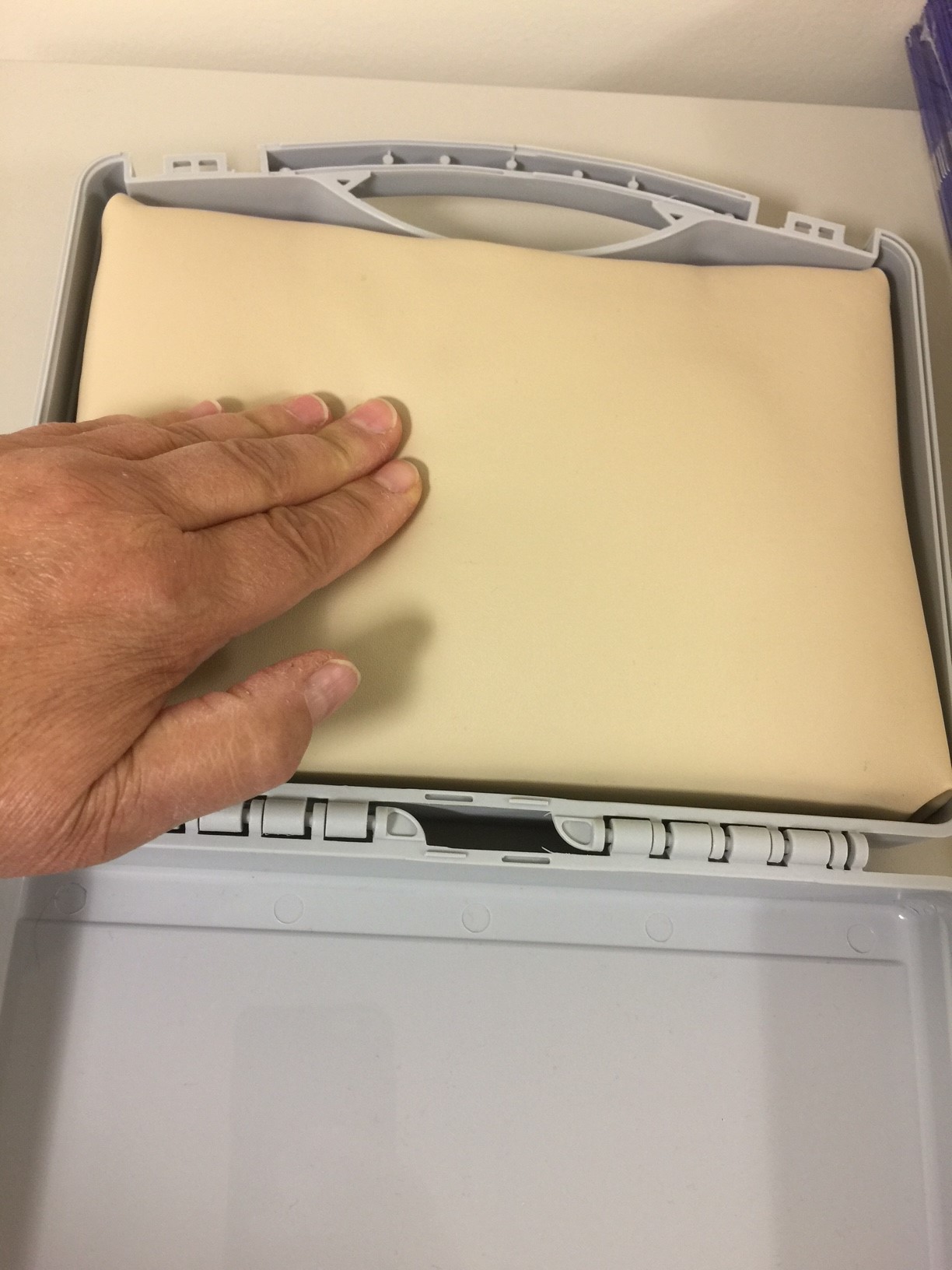
Lipohypertrophy is the development of lumps, raised areas, firmness or hardness in the fatty tissue under the skin caused by the repeated injection or infusion of insulin (a growth factor).
One 2018 study1, like other studies, showed the risk of lipohypertrophy increased with1:
- Inadequate rotation of sites
- Inadequate spacing between injections
- Longer duration of insulin therapy
- Increasing doses of insulin
Although the 2018 FIT5 guidelines note that current evidence does not support the development of lipohypertrophy with GLP-1 receptor agonist injections, these injectables can result in other site irritations or "bumps", depending on the brand and injection technique. Some GLP-1 injectables are now available in weekly doses, thereby reducing any skin irritation simply by reducing frequency.
2. Injection Technique Affects Glycemic Control
Lipohypertrophy can result in unpredictable absorption of insulin (decreased rate or increased variability in rate). This may impact A1c (in one study up to 0.55% higher4), frequency of unexpected hypoglycemia, degree of hyperglycemia, freqency of DKA and total daily dose of insulin.
One study found that structured training on injection technique reduced LH as well as reduced A1c by 1%6. Another study1 showed lipohypertrophy was associated with a 2.7 times higher risk of severe hypoglycemia. As well, this study identified lack of rotation of injection sites, higher daily insulin doses, and (interestingly) keeping insulin in use in the refrigerator as independent correlates of higher HbA1c levels.
Unfortunately, patients often prefer injections into LH sites because they often don't feel the injections (less supply of nerves) or because of shear habit.
3. Suggestions for Lipohypertrophy
The following are suggestions to provide patients or to support patients with LH.- Avoid injections into areas of LH for at least 2-3 months. When switching from an LH site to a new site, a reduction in insuiln may be required to avoid hypoglycemia.
- Educate all patients using insulin on how to check for and prevent LH, especially those with longer duration of insulin therapy. Patients are more likely to rotate correctly if they've received injection review in the past 6 months4. Consider downloading FIT Canada teaching handouts.
- Rotate large injection sites (left upper abdomen, right lower abdomen, buttocks etc)
- Space injections by 1 finger width (1-2 cm) and pump infusion sites by 3 inches (7 cm)
- Change insulin pump sites every 2-3 days or sooner if on large daily doses or sites are irritated.
- Avoid re-using needles
- Consider concentrated insulins for those on large doses
- Inspect injection and infusion sites regularly
References:
1 Pozzuoli, G.M., Laudato, M., Barone, M. et al. Errors in insulin treatment management and lipohyertoprhy. Acta Diabetol (2018) 55: 67. https://doi.org/10.1007/s00592-017-1066-y
2 Blanco M, Hernandez M, Strauss K, et al.Prevalence and risk factors of lipohypertrophy in insulin-injecting patients with diabetes. Diabetes Metab. 2013;39:445-453.DOI: 10.1016/j.diabet.2013.05.006
3 Bertuzzi, F., Meneghini, E., Bruschi, E. et al. Ultrasound characterization of insulin induced lipohypertrophy in type 1 diabetes mellitus. J Endocrinol Invest (2017) 40: 1107. https://doi.org/10.1007/s40618-017-0675-1
4 Frid, A, Hirsch LJ, Menchior AR et al.Worldwide Injection Technique Questionnaire Study
Mayo Clinic Proceedings, 2016; 91(9): 1212-1223. https://doi.org/10.1016/j.mayocp.2016.06.012
5 Forum for Injection Technique (FIT)
6 Misnikova IV, Gubkina VA, Lakeeva TS, Dreval AV. A Randomized Controlled Trial to Assess the Impact of Proper Insulin Injection Technique Training on Glycemic Control. Diabetes Therapy. 2017;8(6):1309-1318. doi:10.1007/s13300-017-0315-y.