The following nutrition guidelines are provided for clinician information and guidance. When talking with patients, remember to use client-centered counselling skills. It's rare that people follow all dietary recommendations.
- Build on current positive habits.
- Involve the patient in setting realistic goals
- Limit the number of lifestyle goals that the patient sets
Safety
Insulin and insulin secretagogues carry a risk of hypoglycemia. To help lower the risk:
- Individualize the amount and distribution of carbohydrate.
- Some people might benefit from moving towards more equal meal sizes.
- Some may benefit from healthy snacks, which may improve glycemic control and reduce hunger and subsequent over-consumption at the next meal. Inclusion of snacks should be individualized and balanced against the potential that we might be promoting weight gain.
- Activity may lower blood glucose levels. If this is an issue for your client, medications might be adjusted, or extra carbohydrate may be consumed.
- Alcohol intake can inhibit gluconeogenesis and the release of glucose from the liver, which may lead to lowered blood glucose levels. Excessive alcohol intake may also impair awareness of hypoglycemia. Hypoglycemia may be delayed by up to 12 hours. Some alcoholic drinks contain carbohydrate that may partially offset the risk, but there's still the potential for a delayed effect (see resources at the bottom of the page).
Encourage patients on insulin or secretagogues to- Avoid excessive alcohol intake.
- In Jan, 2023, new guidelines were adopted by the Canadian Centre on Substance Use and Addiction. They encourage Canadians to have no more than 2 standard drinks per week.
- Ensure that alcohol is not consumed on an empty stomach
- Check blood glucose before bed, after having consumed alcohol
- Accept slightly higher glucose levels after having alcohol
- Avoid excessive alcohol intake.
SGLT-2 inhibitors increase the risk of dehydration, so ensure an adequate fluid intake.
Acarbose (Glucobay) is not used very often in Canada, but it should be noted that it inhibits the digestion of disaccharides. Inform patients on acarbose that treatment for hypoglycemia needs to be glucose, a monosaccharide. Examples include Dextrose tablets or honey.
Healthy Eating
- Everyone is encouraged to eat in a healthy way, and it's no different for people with diabetes. The following abbreviated list describes some of the features of healthy eating. For more information, please refer to Canada's Food Guide.
- Plenty of vegetables and fruits
- Protein foods: have fish twice per week, include plant-based protein alternatives
- Choose whole grain foods
- Limit foods high in sodium, sugar or saturated fat
- Make water your drink of choice
- Enjoy your food
- Cook more often

Body weight
- People who are overweight at diagnosis of type 2 diabetes show improved glucose levels with a loss of 5 to 10% of their initial weight. Unfortunately, current weight loss interventions show poor long-term results and high rates of recidivism. Weight re-gain is less pronounced with bariatric surgery, but this option has limited availability.
- Society promotes unhealthy attitudes toward weight and puts pressure on people to try to achieve an idealized, thin body shape. In people with diabetes, this can contribute to added guilt and disordered eating.
- Weight regulation is complex. It's influenced by many factors. As health care providers, it's important that we don't add to negative messaging around body weight. We can help by:
- Encouraging healthy eating rather than focusing on body weight.
- Avoiding congratulating people on the weight loss they may experience when first diagnosed.
- Avoiding judgment we may inadvertently communicate to patients when they gain weight.
- Alberta Health Services has embarked on a 'Bariatric Friendly Hospital Initiative' described here. To learn more, here are the guidelines for the care of hospitalized patients with bariatric needs.
Meal spacing
- Meal spacing is individualized.
- In general: In type 2 diabetes, recommend well-spaced meals that are fairly consistent in carbohydrate content.
- In people who are taking bolus insulin, match the insulin to the carbohydrate.
- The recommendation for healthy snacks is individualized and balanced against the potential that we might be promoting weight gain.
Portions
Alberta Health Services has several patient resources available for helping to educate people with diabetes. A commonly used one is Healthy Eating for Diabetes. For others, please see this page and look under Diabetes.
A simple guideline for talking about healthy portions, is to consider the happy plate: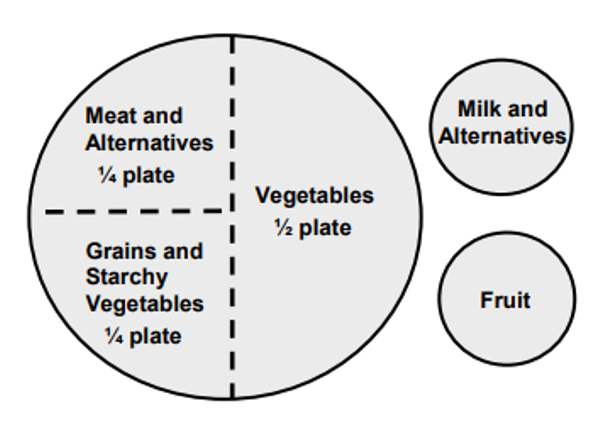
Or the hand jive system, where reasonable amounts for meals equate to approximately the size of:
- One fist for starchy foods, and for fruit
- Two hands full for vegetables

- One palm for meat, fish, or plant-based alternative.
Carbohydrates
Controlling the amount of carbohydrate can help to control blood glucose. There are different strategies that might be used to assist in controlling carbohydrate, from simple to complex. The strategy used is individualized. Visit the Carbohydrate Management page for more information.
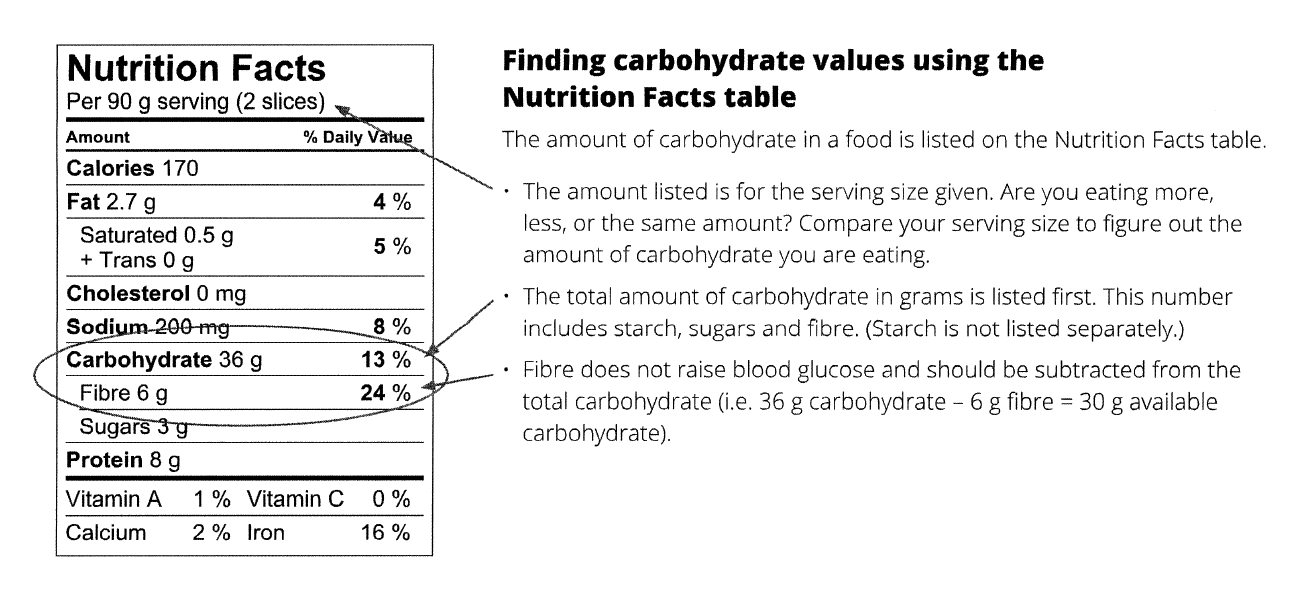
Carbohydrate foods are grouped into portions (referred to as choices) that provide 15 g available carb per serving. Available carb is the carbohydrate that is digested and appears as glucose in the blood. It includes both starch and sugar, but does not include fibre.
A general guideline for the number of carbohydrate choices to eat per meal is 2-4 for most women and 4-6 for most men. For snacks: 0-1 for women and 0-2 carb choices for men.
Examples of foods and portions that count as 15 g available carb include:
125 mL (1/2 c) of potato, corn, pasta or cold cereal
1 medium apple or orange, 1/2 large banana, 250 mL (1 c) blueberries or 125 mL (1/2 c) unsweetened juice
250 mL (1 c) milk or fortified soy milk
15 mL (1 T) honey, sugar or syrup
Looking together with your patient, for nutrition data online, can be a very effective way to highlight the amount of carbohydrate people may not realize are found in foods they are ingesting, for example, specialty drinks. Many flavored coffees and fruit drinks contain 45 to 75 g of available carb (equalling 3 to 5 slices of bread).
Fibre
Foods high in fibre are encouraged to help with glycemic control, as well as other recognized benefits: bowel regularity, improved cholesterol levels and decreased cardiovascular disease risk.
Glycemic index
Low glycemic index foods are encouraged. Glycemic index is a measure of the total effect of a specific carbohydrate food on blood glucose, on a scale of 1 to 100 (lower is better). In general, you may say that the "closer a food is to its whole natural state, the lower the glycemic index."
Sugars and sweeteners
High sugar foods make glycemic control more difficult. The World Health Organization (WHO) recommends <10% of calories from added sugar. For most people this would be no more than 40 to 55 mL (8 to 11 teaspoons) of table sugar. Note that 1 can (350 mL) of regular pop contains 45 to 50 mL of sugar.
Non-nutritive (or artificial) sweeteners have undergone extensive testing and have been found to be safe by Health Canada. Approved artificial sweeteners include:
- Acesulfame potassium (Ace-K)
- Aspartame
- Neotame
- Steviol glycosides
- Sucralose
- Thaumatin (may be added to foods, but not yet available as table top sweetener)
- Saccharin and cyclamate (less common, but still available)
Nutrition resources
- Nutrition guidelines for all clinicians are available at AHS Nutrition Guidelines for Healthcare Providers.
- Detailed guidelines are available to RDs within AHS on the NFS shared drive. Dietitians who work in PCNs have access via Nutrition Services Sharepoint.
- Publicly Available AHS Nutrition Education Materials (Click on Diabetes).
- To learn about options for your patient to see a dietitian, please refer to our listing of Diabetes Services in the Calgary area.
- For more information about the effects of alcohol, see this review article.